The Inhibitory Effect of Thioridazine on adeB Efflux Pump Gene Expression in Multidrug-Resistant Acinetobacter baumannii Isolates Using Real Time PCR
-
Ahmadi , Fereshteh
-
Student Research Committee, Yasuj University of Medical Sciences, Yasuj, Iran
-
Khalvati , Bahman
-
Medicinal Plants Research Center, Yasuj University of Medical Sciences, Yasuj, Iran
-
Eslami , Saba
-
Shiraz University of Medical Sciences, Shiraz, Iran
-
Mirzaii, Mehdi
-
Faculty of Medicine, Shahroud University of Medical Sciences, Shahroud, Iran
-
Roustaei , Narges
-
Department of Epidemiology and Biostatistics, School of Health and Nutrition Sciences, Social Determinants of Health Research Center, Yasuj University of Medical Sciences, Yasuj, Iran
-
Mazloomirad , Farzad
-
Student Research Committee, Yasuj University of Medical Sciences, Yasuj, Iran
-
 Khoramrooz, Seyed Sajjad
Cellular and Molecular Research Center, Yasuj University of Medical Sciences, Yasuj, Iran, Khoramrooz@gmail.com
Khoramrooz, Seyed Sajjad
Cellular and Molecular Research Center, Yasuj University of Medical Sciences, Yasuj, Iran, Khoramrooz@gmail.com
-
Cellular and Molecular Research Center, Yasuj University of Medical Sciences, Yasuj, Iran
-
Department of Microbiology, School of Medicine, Yasuj University of Medical Sciences, Yasuj, Iran
Abstract: Background: The purpose of the present study was to investigate the antimicrobial effects of berberine and thioridazine, as well as their effect on the gene expression of the AdeABC efflux pump system in Multidrug-Resistant (MDR) Acinetobacter baumannii (A. baumannii) isolates.
Methods: This study was carried out in five MDR clinical isolates of A. baumannii and a sample of standard strain (A. baumannii PTCC1797). The effect of Minimum Inhibitory Concentration (MIC) and the Minimum Bactericidal Concentration (MBC) of berberine, thioridazine, and ciprofloxacin alone and their combination on A. baumannii was evaluated by broth microdilution method. Also, their effect on the expression of adeB efflux pump gene was evaluated using real time PCR method.
Results: The MIC of thioridazine, berberine, ciprofloxacin+thioridazine, ciprofloxacin+ berberine, thioridazine+berberine, and ciprofloxacin+thioridazine+berberine on MDR A. baumannii isolates was 64, 256, 128, 256, 128, and 128 μg/ml, respectively. The results showed that treatment of strains with thioridazine alone and in combination with berberine and ciprofloxacin significantly (p<0.05) decreased the expression of adeB efflux pump gene.
Conclusion: Due to the inhibitory effects of thioridazine on bacterial isolates and adeB efflux pump gene, this compound can be used as a potential antimicrobial agent against MDR A. baumannii.
Introduction :
Acinetobacter baumannii (A. baumannii) plays an important role in nosocomial infections 1. This bacterium causes infection and hospitalization , especially in the intensive care unit, burns unit, and surgery wards and increases mortality in people with impaired immune systems 2. Multidrug Resistant (MDR) A. baumannii shows resistance through various mechanisms such as aminoglycoside modifying enzymes, change of outer membrane, biofilm formation, and increased expression of efflux pump 3. Efflux pump is one of the main mechanisms in the development of resistance in A. baumannii 2. One of the most important of these efflux pumps is the AdeABC pump belonging to Resistance-Nodulation-Division (RND) family and one of the main components, called adeB, as a transporter protein, causes antibiotics to be expelled from the bacterial cell 4. Studies have shown that disrupting the efflux pump can increase the antimicrobial properties of antibiotics and biocides against bacteria. In recent decades, the use of herbal medicines and biocides alone or in combination has been widespread to increase the effectiveness of antibiotics 5. One of these phytochemical compounds is berberine, which has several phenolic rings as an isoquinoline alkaloid. According to studies, this substance affects the bacterial cell membrane and disrupts its structure, causing the material to leak out of the cell 6. Another antimicrobial compound used is thioridazine from the phenothiazine family. According to studies, thioridazine, by having a synergistic effect with cloxacillin and miconazole, can reduce the expression of the efflux pump gene in methicillin-re-sistant Staphylococcus aureus (S. aureus) 7. Considering the important role of efflux pumps in antibiotic resistance in Acinetobacter isolates and the possible role of berberine and thioridazine in inhibiting some of these pumps, the purpose of this study was to investigate the antimicrobial effects of these two compounds alone and in combination against MDR A. baumannii and also investigate the effect of these two substances on the gene expression of AdeABC efflux pump system using real time PCR.
Materials and Methods :
Bacterial strains
In this experimental study, 6 strains of A. baumannii including five MDR clinical isolates and a standard strain (A. baumannii PTCC1797) obtained from Iran Scientific and Industrial Research Center were included in the study. A. baumannii isolates were identified using standard biochemical test and finally confirmed by amplification of gltA gene using PCR method.
Determination of the MIC
The antimicrobial effects of the compounds were evaluated by broth microdilution method with the following treatments: group 1 received thioridazine; group 2, berberine; group 3, ciprofloxacin; group 4, thioridazine and berberine; group 5, thioridazine and ciprofloxacin; group 6, berberine and ciprofloxacin; and group 7, thioridazine and berberine and ciprofloxacin. MIC determination was done by broth microdilution method, according to CLSI guideline 8. Then, serial dilution process was administered and dilutions equivalent to 256 μg/ml, 128 μg/ml, 64 μg/ml, 32 μg/ ml, 16 μg/ml, 8 μg/ml, and 4 μg/ml were prepared from thioridazine, berberine, and ciprofloxacin solutions. Also, dilutions in the range of 256 μg/ml to 4 μg/ml were prepared for combinations of each compound. In order to determine the MBC, 10 microliters per well were cultured separately in Mueller–Hinton agar medium in which the bacterium was not grown with 5% sheep blood. Then, incubation at 37°C was done for 18-24 hr, and finally, the lowest concentration of the treatment in which no bacterial growth was observed was reported as MBC concentration 9.
Detection of adeB gene by PCR
Genomic DNA of bacteria was extracted using boiling method 10. PCR amplification was performed in a 25 µl total volume containing 12.5 µl master mix (Amplicon, Denmark), 25 pmol of each primer, and 3 µl of DNA template.
Expression of adeB efflux pump gene by real time PCR
Sediment preparation: The volume required for sedimentation of seven different treatments was calculated according to the MIC concentration in 1 ml of the microtube. All calculations were based on C1V1=C2V2 formula. After calculations, the required volume of each treatment including 100 μl of bacteria grown overnight at a concentration of 107 CFU/ml was poured into a 1.5 ml microtube. Then, the remaining volume of 1 cc was brought to final volume with sterile Mueller–Hinton broth culture medium. After 20 hr of incubation, the microtubes were centrifuged at 15,000 rpm for 10 min. The microtube supernatant was removed and the contents were washed three times with distilled water. The final precipitate was stored at -20°C for further analysis. All of these stages were performed on 7 treatment groups and a control group.
RNA extraction and cDNA synthesis
After sedimentation, RNA was extracted from clinical and standard samples using RNA extraction kit (Pars Toos Company, Iran) according to the instructions. Then, cDNA synthesis was performed using a cDNA synthesis kit (Pars Toos Company, Iran) in one cycle with two different temperatures (37°C for 15 min and 85°C for 5 s).
Quantitative real time PCR method
At this stage, BIO RAD CFX96 was used to quantitatively evaluate the gene expression of A. baumannii. To quantify the expression of the adeB gene, a master mix (containing SYBER Green) was prepared; the volume of the master mix was 20 μl, including 1 μl of each primer, 3 μl of distilled water, 10 μl of buffer, and then 5 μl of cDNA was added to master mix. In this reaction, adeB and rpoB primers were used according to table 1. The rpoB gene was used as an internal control with the ability to be stable in different conditions in order to compare and properly measure gene expression. Finally, the relative expression of adeB gene in A. baumannii isolates was calculated by ΔΔCT method. To calculate the expression of the desired gene by real time PCR (due to SYBER Green use), the relative comparison method (Ct: cycle threshold) was used as follows, relative measurement of Ct=Ct of the desired gene without the presence of intervention-Ct of the desired gene in the presence of the intervention and a fold change of expression=2-ΔCt (Treated –Untreated). A re-ference gene (rpoB gene) as a housekeeping gene was used to normalize the results.
Data analysis
SPSS software v21 (IBM, USA) was used for statistical analysis. The results were analyzed by t-test, one-way analysis of variance, and multiple comparisons. A p-value of ≤0.05 was considered statistically significant.
Results :
The MIC of thioridazine was 64 μg/ml and ciprofloxacin in combination with thioridazine was 128 μg/ ml. The MIC of ciprofloxacin, berberine, thioridazine, ciprofloxacin+berberine, ciprofloxacin+thioridazine, and ciprofloxacin+thioridazine+berberine on MDR A. baumannii isolates is shown in table 2. The Minimum Bactericide Concentrations (MBCs) of ciprofloxacin, thioridazine, berberine, and ciprofloxacin+berberine on clinical isolates of A. baumanii were 256, 128, 256, and 256 μg/ml, respectively.
According to multiple comparison tests, there were significant differences in the expression of adeB gene among different treatments of A. baumanii. In different treatments, the expression of adeB gene decreased in the presence of thioridazine alone or in combination with ciprofloxacin and berberine. The expression of adeB gene in thioridazine group in comparison with the ciprofloxacin, ciprofloxacin+ berberine, and ciprofloxacin+berberine+thioridazine decreased significantly. The results of changing the expression of adeB efflux pump gene by different treatments in A. baumannii strains compared to the control group are shown in figure 1. In clinical isolates and standard strains, after treatment with thioridazine (p<0.000), ciprofloxacin+thioridazine (p<0.031), berberine+thioridazine (p< 0.000), a significant decrease in efflux pump gene expression was observed.
Discussion :
In the present study, it was shown that thioridazine alone and in combination with ciprofloxacin and berberine can cause decreased adeB efflux pump gene expression in A. baumannii strains. In a study conducted by Abdi et al using quantitative real time PCR method, they concluded that peptide nucleic acids (PNAs) reduced the expression level of adeB gene in A. baumannii strain. This may be due to inhibition of translation and transcription of the target gene 12. In a study by Ruzin et al using RT-PCR method, it was shown that there was a significant relationship between the expression of the AdeABC efflux pump gene and the MIC of ethidium bromide 13. In our study, thioridazine in combination with ciprofloxacin and thioridazine in combination with berberine decreased the expression of the adeB efflux pump gene. In a study by Jorgensen et al, the effect of thioridazine T5 derivative on methicillin-resistant Staphylococcus aureus was examined and they concluded that MIC of T5 (1-2 μg/ ml) inhibited bacterial growth. However, in our study, MIC of thioridazine at a concentration of 64 μg/ml inhibited the growth of MDR A. baumannii isolates. This may be due to the use of different thioridazine derivatives or due to the impermeable outer membrane in gram-negative bacteria 14. In our study, thioridazine in combination with ciprofloxacin reduced the MIC. The reason is that thioridazine can reduce ciprofloxacin sensitivity by blocking efflux pumps. Thioridazine may impair its function by binding to the transport structure of the efflux pump 15. In the present study, the effect of berberine alone and in combination with the ciprofloxacin and thioridazine was investigated. According to a study conducted by Mahmoudi et al, it was found that berberine reduced the MIC of imipenem and ciprofloxacin by an average of 0 to 2 fold and 0 to 1 fold, respectively in A. baumanii isolates 6. In our study, berberine in combination with ciprofloxacin reduced the MIC of ciprofloxacin between zero and 2 fold. Agha-yan et al reported that berberine and palmatine reduced the MIC of ciprofloxacin in Pseudomonas aeruginosa, but according to PCR results, no significant correlation was observed between the gene patterns of the efflux pump, MexAB-OprM, and berberine and palmatine 16. According to Jian J et al studies, gram-positive bacteria were more sensitive to berberine than gram-negative bacteria. In our study, berberine alone had no antibacterial effect on A. baumannii, which may be due to an impermeable outer membrane in gram-negative bacteria 5. However, in our study, berberine alone had no inhibitory effect on A. baumannii, which may be due to the use of bacterial strains from different sources or due to the use of different berberine derivatives, which may affect the MIC 17. Thioridazine alone and in combination with berberine and ciprofloxacin can reduce resistance in MDR strains of A. baumannii by reducing the expression of adeB efflux pump gene.
Conclusion :
Due to the inhibitory effects of thioridazine on bacterial isolates and adeB efflux pump gene, this compound can be used as a potential antimicrobial agent against MDR A. baumannii.
Acknowledgement :
This study has been supported by Deputy of Research and Technology of Yasuj University of Medical Sciences.
Ethics Approval :
The study was conducted in accordance with the Declaration of Helsinki. This study has been approved by Research Ethics Committee of Yasuj University of Medical Sciences (IR.YUMS.REC.1399.084).
Conflict of Interest :
The authors declare that they have no competing interests.
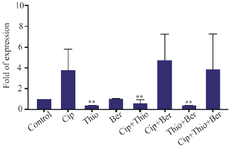
Figure 1. The adeB gene expression of A. baumanii in different treatment groups; treatment with thioridazine, ciprofloxacin+ thioridazine, and thioridazine+berberine significantly decreased adeB gene expression in clinical and standard strains of A. baumanii (Cip: Ciprofloxacin, Ber: Berberine, Thio: Thioredazin).
|
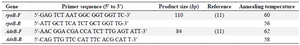
Table 1. The oligonucleotides sequence of primers used in real time PCR reaction in this study
|
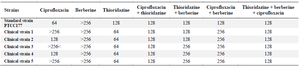
Table 2. The MIC (μg/ml) of ciprofloxacin, berberine, thioridazine on clinical and standard strain of A. baumanii isolates
|
|