Detection of Aneuploidies in Products of Conception and Neonatal Deaths in Iranian Patients Using the Multiplex Ligation-Dependent Probe Amplification (MLPA)
-
Khorami Sarvestani, Sara
-
Fetal Health Research Center, Hope Generation Foundation, Tehran, Iran
-
Reproductive Immunology Research Center, Avicenna Research Institute, Academic Center for Education, Culture and Research (ACECR), Tehran, Iran
-
Rafati, Maryam
-
Fetal Health Research Center, Hope Generation Foundation, Tehran, Iran
-
Reproductive Biotechnology Research Center, Avicenna Research Institute, ACECR, Tehran, Iran, Tehran, Iran
-
Hoseini, Azadeh
-
Fetal Health Research Center, Hope Generation Foundation, Tehran, Iran
-
Soltani, Azadeh
-
Avicenna Fertility Center, Avicenna Research Institute, ACECR, Tehran, Iran
-
Jalilian, Koosha
-
Department of Cellular and Molecular Biology, Faculty of Biological Sciences, Kharazmi University, Tehran, Iran
-
 Ghaffari, Saeed Reza
Reproductive Biotechnology Research Center, Avicenna Research Institute, ACECR, Tehran, Iran, Tel: +98 21 22432020; Email: saeed@ghaffari.org
Ghaffari, Saeed Reza
Reproductive Biotechnology Research Center, Avicenna Research Institute, ACECR, Tehran, Iran, Tel: +98 21 22432020; Email: saeed@ghaffari.org
Abstract: Background: Around 70% of all pregnancies (Including 15% of clinically-recognized ones) are lost due to various fetal or maternal disorders. Chromosomal aneuploidies are among the most common causes of pregnancy loss. Standard chromosome analysis using G-banding technique (Karyotype) is the technique of choice in studying such abnormalities; however, this technique is time-consuming and sensitive, and limited by vulnerabilities such as cell culture failure. The use of molecular cytogenetic techniques, including array-based techniques and Multiplex Ligation-Dependent Probe Amplification (MLPA), has been proposed to overcome the limitations of this method to study the products of conception. This study has been designed to investigate the feasibility of using MLPA technique as a standalone genetic testing, with histopathologic examinations and genetic counseling to detect aneuploidies in products of conception and neonatal deaths.
Methods: Forty-two verified fetal and neonatal samples were studies and genetic counseling was scheduled for all parents. Histopathologic examinations were carried out on the products of conception, and appropriate fetal tissues were separated for genetic studies. Following DNA extraction and purification, MLPA was carried out to investigate chromosomal aneuploidies.
Results: Nine samples (21.42%) were diagnosed to be affected with aneuploidy. Detected aneuploidies were trisomy 22 (n=3), trisomy 21(n=1), trisomy 18 (n=2), trisomy 16 (n=1), trisomy 13 (n=1), and monosomy of chromosome X (n=1). The MLPA analysis results were conclusive for all of the fetal samples (Success rate: 100%).
Conclusion: These results suggest that MLPA, as a standalone genetic testing, is an accurate, rapid, and reliable method in overcoming the limitations of standard cytogenetic techniques in genetic investigation of products of conception.
Introduction :
Approximately 70% of all pregnancies including 15% of clinically detected ones are lost due to various fetal or maternal disorders 1,2. Parents often want to know the reasons for the pregnancy loss. Identifying causes can help determine the aneuploidy recurrence risk in future pregnancies, which is particularly relevant in cases of pregnancy loss. Chromosomal aneuploidy is one of the most common causes of pregnancy loss 3,4.
The metaphase karyotyping is the technique of choice to study common genetic causes of pregnancy loss and neonatal deaths. However, metaphase karyotyping requires cell culture, which leads to long turn-around time for results. Also, there is a risk of gaining no results due to high culture failure rates of 10-40% and the potential for selective overgrowth of maternally derived cells leading to a 46, XX karyotype despite underlying fetal abnormality in 29-58% of cases 5-10.
However, molecular cytogenetic techniques such as Fluorescence In Situ Hybridization (FISH), Quantitative Fluorescence PCR (QF-PCR), Comparative Genomic Hybridization (CGH), and array CGH can detect copy number variations, but they have some limitations. QF-PCR, CGH, and FISH are restricted by the number of target chromosomes that can be analyzed for each assay. Although array CGH as a more comprehensive technique can overcome the limitations, it remains an expensive technique which is not available in several genetic laboratories in Iran. Regarding these facts, perhaps in some instances, Multiplex Ligation-dependent Probe Amplification (MLPA) would be a better alternative to the mentioned techniques for detecting chromosome aneuploidies 9,11-15. This research was carried out to investigate the feasibility of using MLPA technique as a standalone genetic testing, together with histopathologic findings and genetic counseling data, to detect aneuploidies in products of conception and neonatal deaths.
Materials and Methods :
Totally 50 samples of products of conception and neonatal deaths from patients referred to Department of Genetics and Pathology of Hope Generation Foundation and Avicenna Fertility Center were collected for genetic analysis regarding the cause of pregnancy loss or neonatal death. Medical records of each case including screened records were reviewed by a certified genetic counselor. A pathologist conducted internal and external examinations of neonatal deaths; chest and abdominal cavities, the central nervous system, and in some cases, the position of placenta were inspected. Abnormal pathological findings were later cross-referenced with genetic findings. Histopathologic examinations were also carried out on products of conception and neonatal deaths. Eight samples had no embryonic or neonatal tissue, therefore, the remaining forty-two samples were considered for genetic study by a pathologist. This study was performed on thirty-three fetal and nine newborn samples. Collected data set from genetic counseling and histopathologic examinations were entered into the genetic data management system.
A pathologist examined the samples and collected suitable fetal or neonatal tissues for genetic analysis into a sterile falcon tube. Some samples which were paraffin-embedded (2/42) or had a long interval between miscarriage or fetal death until genetic testing (40/42) were sent for MLPA testing as they were not suitable for culture. DNA extraction was performed on cells from 20 mg of tissues using phenol-chloroform DNA extraction method. The concentration and quality of recovered DNA was estimated by NanoDrop 1000 Spectrophotometer (Thermo Fisher Scientific, USA).
MLPA allows the relative quantification of more than 40 sequences in a single multiplex assay using only 20 ng of sample DNA. Denatured genomic DNA was hybridized with a set of two probes, which consisted of a target-specific sequence and a universal forward or reverse PCR primer binding site. One probe had a stuffer sequence to generate various PCR products with different sizes. SALSA MLPA probemix P036B and P070 contained different probes for each chromosome's subtelomeric region and two probes for non-telomeric Y chromosome-specific sequences. After ligation, products were amplified by PCR using only one fluorescent-labeled primer pair. The multiplex-fluorescent products were separated by capillary electrophoresis. The relative amounts of amplified products depended on the quantity of target DNA present in the sample. Therefore, aneuploidy was suspected if probes for both arms of chromosome appeared deleted (Monosomy) or duplicated (Trisomy).
MLPA reaction was performed in a GeneAmp PCR System 9700 (Applied Biosystems, USA) according to manufacturer's instructions. PCR products were electrophoresed in an ABI Prism 3130 Genetic Analyzer and analyzed with GeneMapper software v.4. MLPA peak areas were exported to a Microsoft Excel datasheet to calculate relative peak areas of the amplified probes as a fraction of total sum of peak areas by Coffalyser software v. 9.4.
All procedures were carried out in accordance with the ethical standards of the local committee and the revised version of Declaration of Helsinki in 2013.
Results :
MLPA detected chromosome aneuploidies in 21.42% (9/42) of cases. Typical profiles for normal and abnormal samples are shown in figure 1. All forty-two verified fetal and neonatal samples, which could not be cultured, were analyzed. In general, 95.23% (40/42) of samples were marred by time (Not fresh), and 4.76% (2/42) were paraffin-embedded samples. MLPA gave a conclusive result in all 42 samples. MLPA detected chromosome aneuploidies in 9/42 (21.42%) of cases. These included trisomy 21, 1/9 )11.1%), monosomy X, 1/9 )11.1%), trisomy 18, 2/9) 22.2%), trisomy 13, 1/9 (11.1%), trisomy 16, 1/9) 11.1%), and trisomy 22, 3/9 (33.3%).
Among male fetuses, 79.17% were normal, and among female fetuses, 77.78% were normal. According to Fisher's exact test, there was no difference between normal girls and boys (Table 1).
Distributions of gestational age in total samples were 12/42 (28.57%), from the first trimester, 15/42 (35.71%) the second trimester, 6/42 (14.28%) the third trimester, and 9/42) 21.42%) neonatal samples. When chromosomal abnormalities were analyzed according to the gestational age of the samples, 5/9 (55.55%) of first trimester losses, 3/9 (33.33%) of second trimester losses, and 1/9 (11.11%) of all neonatal deaths with preterm labor in 30 weeks occurred in embryonic specimens with chromosomal abnormalities (Table 2). Data showed no significant difference between gestational age of normal and chromosomally abnormal cases (p=0.090).
The pathological study results in 64.28% of samples (27/42) were available. As shown in table 3, slightly more than half of samples of pregnancy products with normal genetic reports had abnormal findings in the internal or external pathological examination. Of abnormal internal pathologic examinations, 16.66% (7/42) were related to placenta, 7/42 (16.66%) the thoracic cavity, 5/42 (11.90%) the abdominal cavity and 1/42 (2.38%) were associated with central nervous system. Histopathologic exam results included abnormalities in heart tissue 1/42 (2.38%), thymus tissue 1/42 (2.38%), renal tissue 4/42 (9.52%), adrenal tissue 2/42 (4.67%), and liver tissue 2/42 (4.67%). Moreover, all samples with abnormal genetic reports had also been reported as abnormal in histopathology.
In total, 33 and 40% of the patients subjected to first and second trimester screenings, respectively were categorized as cases with high risk of aneuploidy. MLPA method revealed that 40% of cases that underwent screening tests had aneuploidy. Furthermore, abnormal chromosome findings were obtained in a sample with a low risk of aneuploidy.
Discussion :
Prevalence of chromosomal abnormalities in pregnancy has changed the attitude in health systems toward using rapid, accurate, and cost-effective detection methods. This approach could have a significant impact on family health and, subsequently, community's health. Finding causes of fetal or neonatal loss reduces the feelings of self-blame, anxiety, depression, and grief in women with miscarriages or neonatal deaths. Moreover, knowing the exact origin of fetal loss allows us to give improved genetic counseling in future pregnancies to predict the recurrence frequency in each engaged family. Based on these considerations, this study was designed to investigate the feasibility of using MLPA, histopathologic, and genetic counseling data to detect aneuploidies in products of conception and neonatal deaths.
In this study, 50 samples of products of conception and neonatal deaths that could not be cultured, i.e., paraffin-embedded samples or had a long interval between miscarriage or fetal death until genetic testing were evaluated. These samples were collected from Hope Generation Foundation and Avicenna Fertility Center for one year. Based on pathological findings, only forty-two samples contained the fetal or neonatal tissues. Verified samples were analyzed by genetic counseling and MLPA method. Genetic examination was successful in all samples (Failure rate equal to zero), and aneuploidy was detected in 21.42% of samples (Table 4). Aneuploidies included trisomy 18 (22.22%), trisomy 21 (11.11%), trisomy 22 (33.33%), monosomy X (11.11%), trisomy 13 (11.11%), and trisomy 16 (11.11%).
Since 1984, researchers have considered cytogenetic evaluation of products of conception. A review of these studies reveals that culture failure was present in 10-40% of cases. Since 2007, MLPA has been used as a culture-independent method in evaluating those products of conception and neonatal deaths that had no thriving culture 11,12. The results of some studies indicated that MLPA subtelomeric probemix for all chromosomes is the most useful method, especially during the first trimester when numerical aberrations involving all chromosomes may occur 13.
The success rate of MLPA technique in this study is higher than in some similar studies, which could be attributed to smaller sample size 14-16. However, Smits et al conducted a meta-analysis on eight studies that focused on using MLPA in pregnancy loss samples; they reported a 5% failure rate of MLPA 12. Reported aneuploidies in this study have more varieties than similar studies as most of these studies used the SALSA MLPA probemix P095, which is only capable of detecting aneuploidies in chromosomes 13, 18, 21, X, and Y 17-19. However, SALSA MLPA probemix P036 and P070 not only detect subtelomeric rearrangements but also help to study aneuploidies in all chromosomes. However, another study obtained successful MLPA results in only 74.4% of 90 abortus samples while using the SALSA MLPA probemix P036 and P070 20.
Nagashi et al reported 85.3% success rate for karyotype on 407 samples of aborted fetuses in which 61.2% of chromosomal abnormalities were trisomy (Mostly trisomies 16, 21 and 22). They showed that trisomies 7, 8, 14, 15, 16, and 22 were found mostly among the first trimester abortions while trisomies 4, 13, 18, 21 were prevalent in the second trimester 20. In this study, the order of frequency of trisomies was found to be 22: 3/9 (33.3%), 18:2/9 (22.2%), and then 21, 13, 16 each 1/9 (11.1%). Furthermore, in our study, analysis of chromosomal abnormalities (Table 2) shows that there is no significant difference between the gestational age of normal and chromosomally abnormal cases (p=0.090). A larger sample size is required to make a more reliable conclusion.
In 2011, McClelland et al evaluated 382 samples of aborted fetuses and neonatal losses with both MLPA, using SALSA MLPA probemix P069 and P036, and QF-PCR. Seventy-seven reported defects were diagnosed by QF-PCR and the remaining by MLPA. They concluded that with this approach, only 4% of chromosomal aberrations were not detectable, compared to 20-30% failure rate of karyotype analysis. Considering the fact that QF-PCR can only identify common aneuploidies (Trisomy 13, 18, 21, X, Y), MLPA seems a more reasonable approach for the concurrent investigation of such abnormalities together with other aneuploids 21. In this study, 88.88% of aneuploidies were identified as trisomy and 11.11% as monosomy. Ttrisomy 22 was the most frequent aneuploidy detected.
In line with this study, Zimowski et al in 2016 carried out 181 MLPA analyses using subtelomeric and subcentromeric probe kits (SALSA P070 and SALSA P181) on products of first trimester spontaneous miscarriage. As expected, they reported that the differentiation between simple trisomies and trisomies caused by Robertsonian translocation is not feasible 22. In our study, all parents had genetic counseling before the test, and if they had a history of miscarriage, parents' karyotypes were also investigated. The rate of consanguinity between families in this study was 45%, which is in line with the 38.6% consanguinity rate within Iranian families reported by Saadat et al 22.
Careful pathologic examination of the products of conception can help the process of clinical diagnosis, particularly unexpected anomalies and may influence the clinical care, family planning, genetic counseling, and grief management 23. Stuppia et al demonstrated the broad spectrum of MLPA applications in different fields such as detection of neuromuscular disorders, analysis of SHOX gene, prenatal diagnosis, and cancer. Since through MLPA, a large number of genes can be analyzed by a single technique, they argued that MLPA can even be the gold standard for analysis of copy number variation pathologies 24. About 54% of samples with normal genetic report had an abnormal report in the internal or external pathological examination, which were not strictly associated with aneuploidies. On the other hand, all samples with the abnormal genetic report were also reported as abnormal cases pathologically.
Conclusion :
A comprehensive approach using genetic counseling, histopathologic examination, and genetic testing is mandatory to address the possible genetic causes for abortion and neonatal death. In this regard, MLPA as a standalone genetic testing is an accurate, rapid, and reliable method with a low failure rate to overcome the limitations of standard cytogenetic techniques. Moreover, in certain and well selected conditions, this technique may be considered as an alternative to array-based techniques when resources are limited.

Figure 1. Typical profiles for normal and abnormal samples. A) Table A shows the normal female data analysis of MLPA products for SALSA P070 using Coffalyser software. B) Table B represents the male, trisomy 18 data analysis of MLPA product for SALSA P036 using Coffalyser software. C) Electropherogram showing MLPA product for SALSA P036 in Gene Mapper software, arrows marking 18p, and 18q peaks, respectively (47, male, trisomy 18).
|
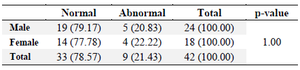
Table 1. Distribution of gender in samples
Fisher's exact test
|
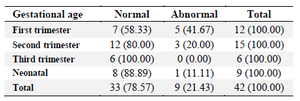
Table 2. Distribution of the gestational age in total samples
|
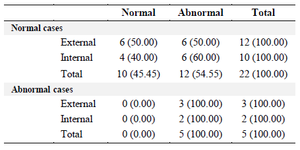
Table 3. Distribution of normal and abnormal pathological reports (Internal and external exam) in total samples
|
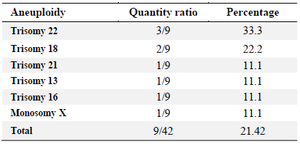
Table 4. Distribution of aneuploidy in total samples
|
|