Evaluation of Seroconversion Rate Following SARS COV 2 Vaccination in Health Care Workers at Shahid Beheshti University of Medical Sciences
-
Mousavi, Mohammad
-
Dentofacial Deformities Research Center, Research Institute of Dental Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
-
Jazayeri, Mohammad
-
Department of Virology, School of Public Health Research Center for Clinical Virology, Tehran University of Medical Sciences, Tehran, Iran
-
 Ebadifar, Asghar
Department of Orthodontics, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran, Tel: +98 21 26708362; Fax: +98 21 22403194; E-mail: a.ebadifar@sbmu.ac.ir
Ebadifar, Asghar
Department of Orthodontics, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran, Tel: +98 21 26708362; Fax: +98 21 22403194; E-mail: a.ebadifar@sbmu.ac.ir
Abstract: Background: Vaccines are the most effective way to prevent Coronavirus 2 severe acute respiratory syndrome (SARS-CoV-2). This study examines and compares the efficiency of AstraZeneca, Sinopharm, and Sputnik vaccines and the correlation of antibody response with age, sex, and history of corona disease in employees of Shahid Beheshti University of Medical Sciences.
Methods: 202 participants were included, of which 82 were administered the AstraZeneca, 59 were given the Sinopharm, and 61 were given the Sputnik vaccine. SARS-CoV-2 IgM and IgG antibody levels were checked four weeks after passing the second dose of all three vaccines using the enzyme-linked immunosorbent assay (ELISA) technique.
Results: There was no significant difference between the amount of IgM and IgG antibodies among three vaccines (p=0.056). For all three vaccines, gender and age did not significantly affect the amount of IgM and IgG antibodies. The history of infection with COVID-19 increased the antibody response (p>0.5).
Conclusion: The titer of IgM and IgG antibodies were not statistically significantly different. The IgM and IgG antibodies produced by vector-based vaccines are higher than the Sinopharm vaccine. Gender did not affect the produced antibody titer. No significant linear relationship was found between age and antibody titer. In people from this study who received two doses of the AstraZeneca vaccine and had a corona history, the average amount of both IgM and IgG antibodies was measured more than the other participants.
Introduction :
Three novel coronaviruses, Coronavirus Associated Severe Acute Respiratory Syndrome (SARS-CoV), Middle East Respiratory Syndrome Coronavirus (MERSCoV), and Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), is a human-to-human transmitted and global pandemic disease 1. SARS-CoV-2 is an enveloped single-stranded positive-sense RNA virus that caused the pandemic of coronavirus disease 2019 (COVID-19) and resulted in millions of deaths across the globe 2. The genome of SARS-CoV-2 is almost 30 kb which encodes major structural proteins, including spike (S) protein and accessory proteins (ORF 3a, 6, 7a, 7b, 8, and 10) 3. The S protein is essential for the life cycle of SARS-COV-2 and is considered a major target antigen for vaccines against the virus. In the host cells, the spike protein is cleaved into S1 [Receptor-Binding Domain (RBD)- containing] and S2 (non-RBD-containing) subunits 4.
In most communities, Healthcare workers (HCWs) are exposed to the virus at a greater level than any other society members and may be considered at an elevated risk of infection. Their role in the chain of transmission is essential, through which they help control and prevent the spread of COVID-19 disease 5.
Various forms of vaccine candidates targeting SARS-CoV-2 are classified as inactivated virus vaccines (Sinovac Biotech, Beijing, China; Sinopharm Beijing Institute of Biotechnology, Beijing, China; Bharat Biotech, Hyderabad, India), Ad26- based vector vaccine (Janssen/Johnson & Johnson, Titusville, NJ, USA), the chimpanzee adenovirus vector vaccine (AstraZeneca, Cambridge, UK/Oxford University, Oxford, UK), Ad5 and Ad26-based vector vaccine (Gamaleya, Moscow, Russia), protein subunit based vaccines (Novavax), and mRNA vaccines (Moderna, Cambridge, US/NIAID, MA, USA; Pfizer, New York, NY, USA/BioNTech, Mainz, Germany) 6,7.
COVID-19 vaccinations induce adaptive protective immunity, including specific T cell and B cell antibody responses 8. Specific antibodies such as IgM, IgG, and IgA mainly bind to the spike protein and can neutralize the fusion and entry of SARS-CoV-2 to the host cell. Therefore, these antibodies form the 'immunological memory' and could aid in preventing the potential COVID-19 virus. The serum concentrations of these antibodies can be analyzed to assess the efficiency of different types of vaccines 9, in this research. We aimed to examine and compare the efficiency of Sputnik, AstraZeneca, and Sinopharm in terms of the amount of antibody produced and the correlation of antibody response with age, sex, and history of corona disease in professors, students, and staff of Shahid Beheshti School of Dentistry and employees of Shahid Beheshti University of Medical Sciences.
Due to the fact that the response of the immune system in different races and human populations is diverse, therefore, conducting this study in an acceptable population in Tehran emphasizes the importance of the work and its novelty.
Materials and Methods :
The Sinopharm vaccine was given to 59 adults in two doses (BBIBP-CorV) (34 females and 25 males, mean age of 38.91 years) and 82 individuals who had been vaccinated with the two doses of the AstraZeneca (ChAdOx1 nCoV-19) (62 females and 20 males, mean age of 42.86 years) and 61 individuals who had been vaccinated with the two doses of the Sputnik (Gam-COVID-Vac) (39 females and 22 males, mean age of 39.77 years) were enrolled in this study. From each volunteer, 5 ml of fresh blood was sampled to prepare serum or plasma. Patients’ information was recorded and consent was obtained from the participants for sampling and all procedures. This study was approved by the Ethics Committee of the Faculty of Dentistry of Shahid Beheshti University of Medical Sciences with the ethics code IR.SBMU.DCR.REC.1400.178.
Inclusion and exclusion criteria: We included individuals who had received two doses of the Sinopharm vaccine (BBIBPCorV), Sputnik (Gam-COVID-Vac), or the AstraZeneca (ChAdOx1 nCoV-19) COVID-19 vaccines. A history of COVID-19 infection that was confirmed, as well as present COVID-19 infection, were both exclusion criteria, in addition to a history of infections with hepatitis viruses and HIV, people with autoimmune disorders and malignancies, those with a history of allergies or anaphylaxis, those immunocompromised, those taking corticosteroids, and the ones taking immunosuppressing drugs.
Laboratory testing: After collecting venous blood samples from the people, SARS-CoV-2 neutralizing antibody (SARS-CoV-2 IgM antibody) and SARS-COV-2 anti-RBD IgG levels (SARS-CoV-2 IgG antibody) (Pishtaz Teb Diagnostic, Tehran, Iran) were evaluated in serum using the Enzyme-Linked Immunosorbent Assay (ELISA) technique according to the company's specifications. Indirect and competitive ELISA measured SARSCoV-2 anti-RBD IgG and SARS-CoV-2 blocking antibody levels, and the results were expressed in relative units RU/ml and μg/ml, respectively.
Statistical analysis: Descriptive statistical methods such as tables, graphs, and statistical indices were used to describe the results. Analyzes were done using SPSS 26 software. The Shapiro-Wilk test was used to check the normality of data distribution. Due to the non-normal distribution of the data, ANCOVA and Kruskal-Wallis trials were used to compare the amount of IgM and IgG antibodies and the efficacy of vaccines. The Mann-Whitney test was used to compare the effect of gender in each vaccine and the impact of a history of corona disease on the increase or decrease of IgM and IgG antibodies. Regression and Scatter analysis were used to check a specific and significant relationship, including a linear relationship between age and antibody response. Statistics were considered essential for the p-values under 0.05.
Results :
The comparison of SARS-COV-2 anti-RBD IgG antibody and neutralizing antibody level: The comparison of SARS-COV-2 anti RBD IgG after the first and the second dose of vaccines showed that the median serum levels of anti-RBD IgG and neutralizing antibody were higher in Astra Zeneca (AstraZeneca > Sputnik > Sinopharm) but the differences were not significant (IgM-p=0.214. respectively, Table 1) (IgG-p=0.056. respectively, Table 2). The units of values in the tables are µg/ml.
Correlation of the antibody titer with SEX: In all three vaccinated groups, the levels of SARS-CoV-2 neutralizing antibody and anti-RBD IgG antibody were not associated with the gender of the participants, and no significant correlation was observed (for IgM, Sputnik p=0.430-AstraZeneca p=0.816-Sinopharm p=0.297 respectively, Figure 1) (for IgG, Sputnik p=0.110-Astrazeneca p=0.548-Sinopharm p= 0.454. respectively, Figure 2).
Correlation of the antibody titer with age:In all three vaccinated groups, the SARS-CoV-2 neutralizing antibody and Anti-RBD IgG antibody levels were not associated with the age of the participants, and no linear correlation was observed (for IgM, Sputnik p=0.853-AstraZeneca p=0.734-Sinopharm p=0.633 respectively, Figure 3) (for IgG, Sputnik p=0.535-Astrazeneca p=0.563-Sinopharm p=0.834 respectively, Figure 4).
Correlation of the antibody titer with prior infection: The history of infection with COVID-19 within six months before the measurement of antibodies increased the antibody response. This increase in response was significant for the AstraZeneca vaccine, but not significant for the other two vaccines (for IgM, Sputnik p=0.940-AstraZeneca p=0.017-Sinopharm p=0.376 respectively, Figure 5) (for IgG, Sputnik p=0.552-AstraZeneca p=0.0001-Sinopharm p=0.281 respectively, Figure 6).
Discussion :
COVID-19 is still an ongoing global pandemic, and the world needs to be immunized against the virus with a vaccine to bring this pandemic to an end 10. Following SARS-COV-2 infection, adaptive immunity generates the receptor binding domain neutralizing antibodies of the spike protein and nucleocapsid protein. In addition, most COVID-19 vaccines trigger neutralizing antibodies specific to the spike protein 11. Vaccination is considered a crucial strategy to control viral infections 12. Corona vaccines use structures similar to the spike protein of the virus. They prepare the immune system to identify the virus 13,14. In glycoprotein S, there is a place called the Receptor Binding Domain (RBD) through which the virus binds to its receptor on the host cell's surface 13-15. Changes in this region are primarily responsible for binding to the Angiotensin-converting enzyme 2 (ACE2) receptor 15.
To measure the level of immunity obtained from corona vaccine, the amount of specific IgG antibodies in the blood is checked 16-18. Neutralizing antibodies cause changes in the spike protein structure and the IgG antibody specifically targets the S1 subunit of the S protein and the RBD. According to the findings of this study, the amount of IgM and IgG antibodies produced as a result of vaccination was the highest in AstraZeneca, but there was no significant difference and the type of vaccine had no significant effect on the amount of antibodies. The amount of IgM and IgG antibodies produced by vector-based vaccines, AstraZeneca and Sputnik, is higher than the Sinopharm vaccine, produced using inactivated virus technology. A study showed that the amount of specific anti-spike IgG produced after the injection of AstraZeneca and Sputnik V vaccines was almost the same 19. Another study showed that the performance of the Sinopharm vaccine in creating anti-spike IgG is weaker than AstraZeneca and Sputnik vaccines 20. According to the results of another study compared to AstraZeneca and Pfizer vaccines, Sinopharm and Sputnik V vaccines produced lower amounts of antibodies and had lower anti-RBD-ACE2 activity 21,22.
According to the results of this study, the amount of IgM and IgG antibodies produced as a result of vaccine injection was equal in both sexes, and no statistically significant difference was observed. A study showed no meaningful relationship between gender and IgG titer after vaccination in any Sinopharm and AstraZeneca vaccines 21. Another study showed no statistically significant difference in IgG antibody titer in men and women who received AstraZeneca and Sinopharm vaccines 23.
This study observed no clear and significant pattern between age and the amount of IgM and IgG antibodies produced, including a linear relationship. A negative correlation between age and neutralizing IgM antibodies was shown in a study regarding Sinopharm and AstraZeneca vaccines 23. Another study showed that the amount of anti-COVID IgG antibody produced was similar in adults aged 19 to 24 who received the AstraZeneca vaccine, but the titer of SARS-CoV-2 anti-spike IgG was lower in people over 60 receiving this vaccine 24,25.
Individuals with a history of corona disease are expected to have a more robust antibody response after vaccination 26. This study has shown that the history of infection with COVID-19 within six months before the measurement of antibodies increased the antibody response. This increase in response was significant for the AstraZeneca vaccine, but not significant for the other two vaccines. For all three vaccines, the average amount of IgM and IgG antibodies was higher in people with a history of corona disease than those who did not have an account of this disease. This difference in the amount was more remarkable for people from this study who received two doses of the AstraZeneca vaccine than those who received two doses of the Sinopharm and Sputnik vaccines. A study showed that the history of corona disease significantly affected neutralizing antibody titer and IgG antibody titer in both types of AstraZeneca and Sinopharm vaccines 27.
Conclusion :
Our findings point to greater quantitative efficiency of the vector-based AstraZeneca and Sputnik COVID-19 vaccine over the classic inactivated Sinopharm. Our study suggests that booster vaccination is needed for subjects who have had the Sinopharm (BBIBP-CorV) vaccine and people who have had a history of corona disease before. It is better to inject the AstraZeneca vaccine.
Acknowledgement :
We thank the participants for their patience and sincere help. We also thank the field workers who worked hard to collect data and specimens from the participants.
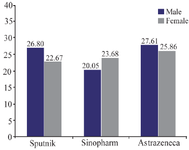
Figure 1. Average amount of IgM antibody for all three vaccines according to gender.
|
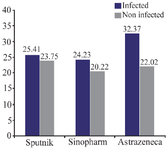
Figure 2. Average amount of IgG antibody for all three vaccines according to gender.
|
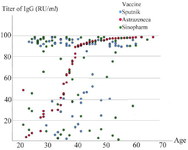
Figure 3. Scatter diagram of the relationship between IgM antibody titer and age.
|
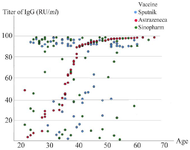
Figure 4. Scatter diagram of the relationship between IgG antibody titer and age.
|
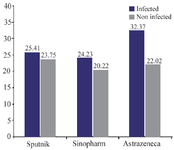
Figure 5. The average amount of IgM antibody for all three vaccines according to the history or lack of the previous infection with corona disease.
|
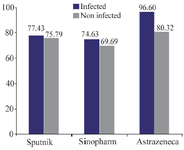
Figure 6. The average amount of IgG antibody for all three vaccines according to the history or lack of the previous infection with corona disease.
|
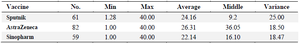
Table 1. Information about IgM antibody response
The units of values in the tables are µg/ml.
|
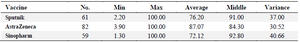
Table 2. Information about IgG antibody response
The units of values in the tables are µg/ml.
|
|